Application and Policy Statuses
Learn the steps to view your application and policy statuses on the website, as well as information about letters you may receive that are related to your application and enrollment.
Application and Policy Status
View My Coverage allows you to view the statuses of your applications and policies once you’ve started the application process. You can view your plans’ statuses on the website.
Complete the following steps:
1. Sign into Via Benefits and select View My Coverage in the Applications and Policies section.
2. On the Policies page, select the name of the person whose applications or policies you want to view.
3. The page shows any submitted applications and any issued policies.
This example shows Jack doesn’t have any applications or policies. He would select Shop for a plan to get started.
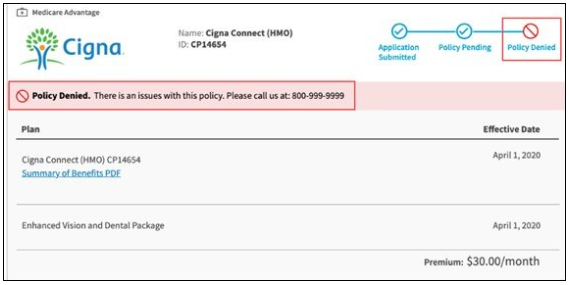
4. For each application or policy, the following information is provided:
Plan type (Medicare Advantage, Dental, Vision, etc.)
Progress tracker shows the status of your application (Application Submitted, Policy Issues, Policy Denied, etc.) You can select underlined words for more information
Plan Name and ID
Link to the Summary of Benefits
Effective Date
Monthly Premium
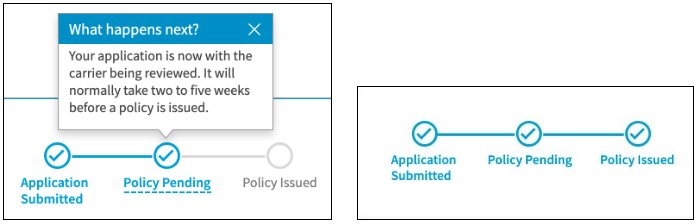
Progress Tracker
The progress tracker begins when you submit your application.
At each stage you can click on the dashed line for more information. Once your application is with the insurance carrier, the progress moves to Policy Pending and, finally, to Policy Issued.
If there's trouble along the way, such as the policy being denied, you're informed.
Note: If two applications are submitted on the same day, the insurance carrier may process them at different times. For example, if you and your spouse apply for the same prescription drug plan on the same day, you may find one application is approved by the carrier, while the other is still pending. Different processing times may result in one person receiving Insurance ID cards and membership information before the other.
Letters
Confirmation of Medicare Information
Generally, receiving a Confirmation of Medicare Information Letter means one or more pieces of personal information on your insurance application didn't match the information on file with Medicare. Carefully read the letter, don't discard it. Action on your part is required and time sensitive. Contact Via Benefits for assistance. Any of our customer service representatives are able to assist you.
Enrollment Confirmation
An enrollment confirmation letter from your insurance carrier verifies receipt of your application and lets you know it's in process. This doesn't necessarily indicate your policy has been issued. Please read the letter carefully to determine if the insurance carrier is asking you to confirm your enrollment via mail or phone. If so, confirm your enrollment as instructed in the letter.
Selection Confirmation
You may also receive a Selection Confirmation Letter from Via Benefits Insurance Services approximately two weeks after completing your enrollment. This letter verifies your application is complete and was sent to the insurance carrier for processing. It doesn't indicate your policy has been issued. The letter also indicates whether Automatic Premium Reimbursement is supported by your plan. If Automatic Premium Reimbursement is supported, the letter indicates whether it’s currently turned on or off.
If you're enrolled in a Medicare Supplement Insurance (Medigap) policy, the letter provides the quoted premium amount. Remember, the quoted premium amount may differ slightly from the final premium amount provided by the insurance carrier.
Contact Via Benefits if you're receiving any request for information from the insurance carrier with which you applied. Not responding within the allotted time frame may cause your application to be denied.